Interesting Case of Systemic Lupus Erythematosus With APS Nephropathy

Case Summary
A 32 year old lady presented with fever, polyarthralgias and fatigue for a duration of 4 months. She was evaluated elsewhere initially, was told to have Anemia and received 9 units of blood transfusions during this period, her lowest blood hemoglobin being 5 g/dl.
She presented to the Rheumatology OP at Yashoda Hospitals when there was no improvement in fever and had developed burning parasthesias and pain in both hands and feet. In the past, she had 2 abortions, one spontaneously during the 1st trimester and the second during the 5th month of gestation due to poor foetal growth.
On examination, she had violaceous and erythematous non- specific rash over upper and lower limbs. Her blood pressure was 100/80 mm of Hg. Systemic examination was unremarkable. Investigations revealed hemoglobin of 10 g/dl, leukocyte count of 4800/cu mm, platelets 2.0 lakh/cu mm, positive coombs (both direct and indirect), ANA profile was positive for DS DNA, Nucleosomes and Histone and Mi2. HerAnti-cardiolipin antibodies was 2 times the upper limit of normal levels, complements (C3 and C4) were low, baseline PT, aPTT and Lupus anticoagulant was Her urine examination revealed trace protein with 4-5 pus cells, serum creatinine of 1.3mg/dl, blood urea in normal range with 24 hour urine protein of 182 mg. Routine cardiac evaluation revealed severe MR. With these findings diagnosis of SLE with Antiphospholipid Antibody Syndrome (APS), Libman- Sacks Endocarditis, Vasculopathy, Hacmolytic Anemia and possible Nephropathy was made.
During this evaluation, she was initiated on 1mg/kg body weight of steroids, low dose diuretic as per cardiologist advice, supportive treatment. But there was no significant improvement, she continued to have the burning parasthesias and also her repeat creatinine increased to 1.5mg/dl, normal blood urea without any active urinary sediment and hypertension.
She was admitted and started on pulse methyl prednisolone 1gm/day for 3 days along therapeutic anticoagulation. A Nephrology consultation was taken and renal biopsy was done. She improved after pulse therapy and patient was discharged pending biopsy report on steroids, antiplatelets and supportive therapy.
Renal biopsy revealed features suggestive of Membranous Nephropathy with Focal Endocapillary Proliferation, activity 4/24 and chronicity 3/12 along with Thrombotic Microangiopathy and Focal Global Glomerulosclerosis, immunoflourescence studies showing Glomerular and Mesangial deposits of IgG, IgM, C3c and C1q with minimal IgA( Figures 1-4). Her serum creatinine improved to 1.2mg/dl by this time.
A diagnosis of SLE with APS, with Autoimmune Hemolytic Anaemia, Libman-Sacks Endocarditis and Lupus Nephritis with APS Nephropathy was made. In consultation with Nephrologist, she was initiated on pulse cyclophosphamide therapy, oral anticoagulants, 1mg Kg BW steroids, ACE inhibitor and supportive treatment. Patient was stable on her last visit and is stable on follow up.
Discussion
This is an interesting case, where a high index of suspicion and a timely renal biopsy helped in making a diagnosis of SLE-APS nephropathy, where the only indication of renal involvement was elevated S.Creatinine, without any active urinary sediment or proteinuria.
Apart from her serology, that is positive for nucleosome and ds DNA antibodies, which together are 99% specific for SLE, all her clinical manifestations including AIHA, Libman-Sacks endocarditis and ischemic pains of the extremities could have been explained by Antiphospholipid Antibody Syndrome.
APS Nephropathy is a rare entity. Diagnosis is usually made when kidney biopsy is done for managing Lupus Nephritis. There are no set indications for kidney biopsy in APS patients, but to be suspected in cases presenting with isolated hypertension, nephritic presentation without any active urinary sediment or in setting of Catastrophic Antiphospholipid Antibody Syndrome.
Management of APS Nephropathy with or without SLE is debatable as there are very few case reports. Anticoagulation is the mainstay of treatment in APS Nephropathy. In SLE with APS Nephropathy most common strategy i s immunosuppression along with anticoagulation to maintain an INR between 2.0 and 3.0. Immunosuppression can be with Cyclophosphamide, Mycophenolate mofetil, Tacrolimus or Rituximab. Plasmapheresis and/ or IVIG along with pulse methyl prednisolone should be considered in setting of RPGN like presentation or when associated with CAPS. Sincere thanks to:
Dr. Sai Ram Reddy, Consultant Nephrologist, and his team, Yashoda Hospitals, Somajiguda.
Dr. Anusha Kumari, Pathologist, Yashoda Hospitals, Secunderabad.
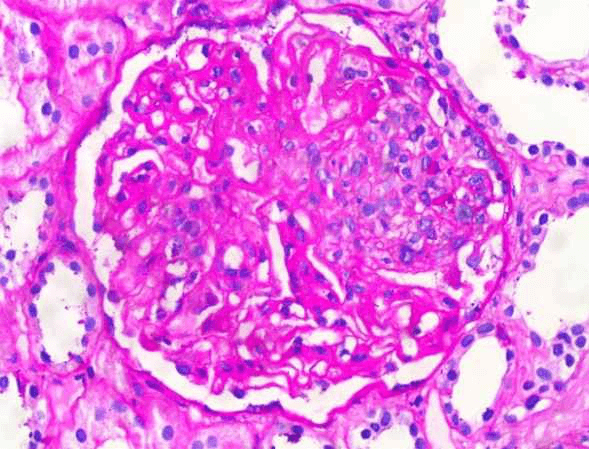
Glomerus with diffuse masement membrane thickening with segmental endocapillary proliferation causing luminal occlusion (PAS, 20X)
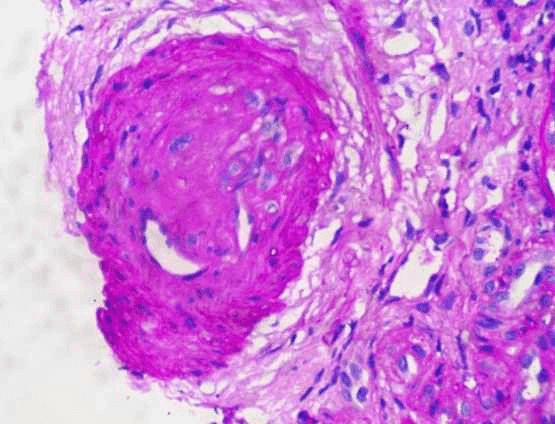
Artery with luminal occlusion due to a thrombus displaying partial recanalization (PAS, 40X)
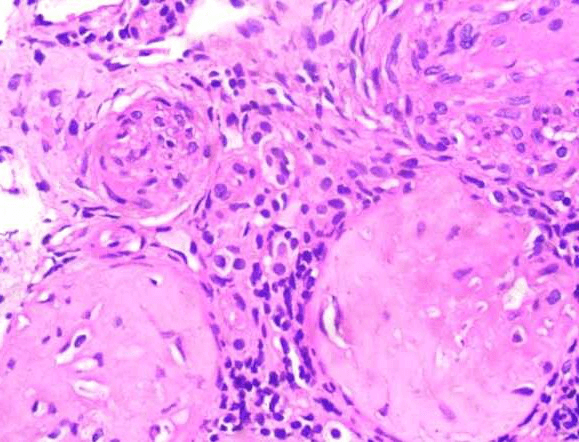
Two sclerosed glomeruli with an artery showing luminal occlusion due to fibrointimal hyperplasia
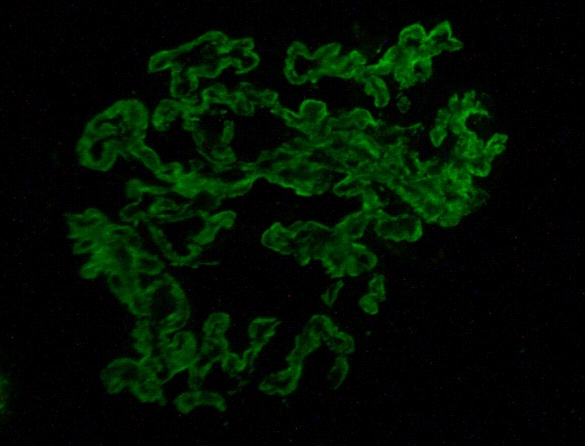
IF showing C1q which shows significant peripheral and focal mesangial immune deposits (IgG, IgM, C3c not shown)
About Author –
Dr. I. Rajendra Vara Prasad, Consultant Rheumatologist, Yashoda Hospitals, Hyderabad
MD, DM (Rheumatology), APLAR Fellowship, Centre for Rheumatology, UCL, London, UK.
His expertise includes systemic lupus erythematosus, myositis & rheumatological emergencies, musculoskeletal & autoimmune diseases in adults and children.